Lithium is a well-known cause of nephrogenic diabetes insipidus (NDI), a condition where the kidneys fail to respond to antidiuretic hormone (ADH, vasopressin), leading to an inability to concentrate urine. Below, I’ll explain the mechanism, clinical features, diagnosis, and management of lithium-induced NDI, with concise details relevant to your query.
Mechanism of Lithium-Induced Nephrogenic DI
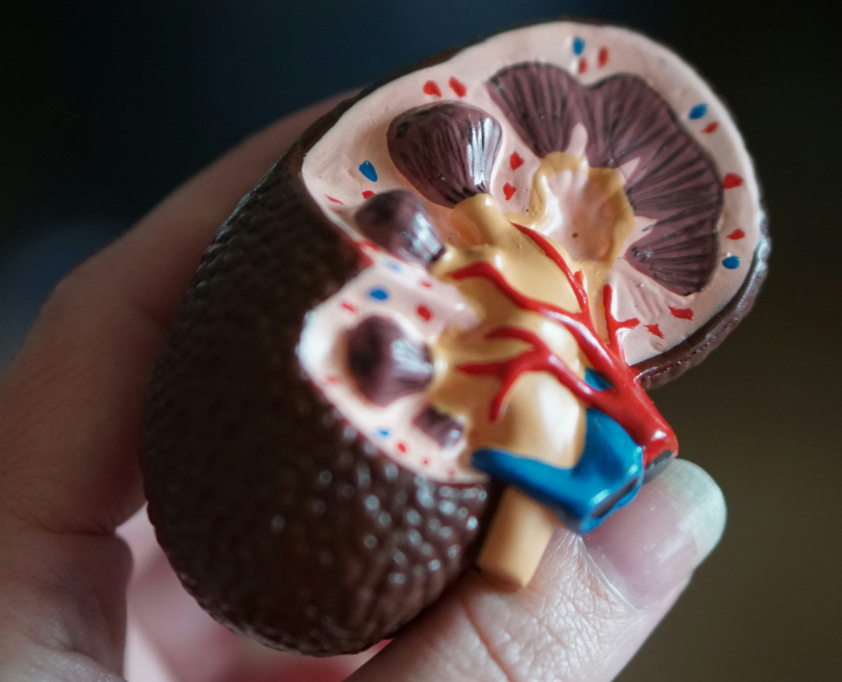
- Primary Effect: Lithium interferes with the vasopressin V2 receptor signaling pathway in the collecting tubules of the kidney.
- Lithium enters renal principal cells via sodium channels (ENaC) and inhibits adenylyl cyclase, reducing cyclic AMP (cAMP) production.
- This impairs the insertion of aquaporin-2 (AQP2) water channels into the apical membrane, preventing water reabsorption.
- Chronic Effects: Prolonged lithium use (>1–2 years) can cause structural damage:
- Downregulation of AQP2 expression.
- Tubulointerstitial fibrosis and chronic kidney disease (CKD), worsening NDI.
- Result: The kidneys cannot concentrate urine, leading to polyuria, polydipsia, and risk of dehydration.
Clinical Features
- Symptoms:
- Polyuria: Large volumes of dilute urine (>3 L/day).
- Polydipsia: Excessive thirst due to water loss.
- Nocturia: Frequent urination at night.
- Dehydration: If fluid intake is inadequate, leading to hypernatremia, fatigue, or confusion.
- Onset:
- Can occur within weeks of starting lithium but is more severe with long-term use.
- Prevalence:
- ~20–40% of lithium-treated patients develop some degree of NDI; severe cases are less common.
Diagnosis
- Clinical History:
- Confirm lithium use (typically for bipolar disorder or mood stabilization).
- Assess duration and dose (higher cumulative exposure increases risk).
- Lab Findings:
- Urine: Low urine osmolality (<300 mOsm/kg), high urine volume.
- Serum: Normal or elevated sodium (hypernatremia if dehydrated), normal or slightly reduced eGFR in chronic cases.
- Serum lithium levels: Therapeutic range (0.6–1.2 mmol/L) can still cause NDI; toxicity (>1.5 mmol/L) worsens it.
- Water Deprivation Test (if needed):
- Differentiates NDI from central DI or primary polydipsia.
- In NDI: Urine osmolality remains low (<300 mOsm/kg) despite water deprivation, and no response to exogenous vasopressin (desmopressin).
- Rarely needed in clear lithium-related cases.
- Rule Out Other Causes:
- Other drugs (e.g., demeclocycline, amphotericin B).
- Genetic NDI, hypercalcemia, hypokalemia, or CKD.
Management
- General Measures:
- Monitor Fluid Balance: Ensure adequate water intake to match urine output and prevent dehydration.
- Serum Sodium: Check regularly to detect hypernatremia early.
- Lithium Review: Assess if lithium can be reduced or discontinued (in consultation with psychiatry, as abrupt cessation may worsen mood disorders).
- Pharmacologic Interventions:
- Amiloride:
- A potassium-sparing diuretic that blocks ENaC, reducing lithium entry into principal cells.
- Dose: 5–10 mg/day.
- Reduces polyuria and protects against lithium toxicity.
- Thiazide Diuretics (e.g., Hydrochlorothiazide):
- Paradoxically reduce urine output by causing mild volume depletion, which enhances proximal tubule water reabsorption.
- Dose: 12.5–25 mg/day.
- Monitor for hypokalemia and hyponatremia.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) (e.g., Indomethacin):
- Increase AQP2 expression and reduce polyuria.
- Use cautiously due to risk of worsening renal function, especially in lithium-induced CKD.
- Desmopressin: Ineffective in pure NDI but may help in partial NDI cases (rare).
- Amiloride:
- Discontinuing Lithium:
- NDI may persist after stopping lithium, especially with chronic use, due to irreversible tubular damage.
- Gradual tapering is preferred to avoid psychiatric decompensation.
- Monitoring:
- Regular renal function tests (eGFR, creatinine).
- Urine osmolality and volume to assess NDI severity.
- Psychiatric follow-up if lithium is adjusted.
Complications
- Dehydration and Hypernatremia: Can lead to confusion, seizures, or coma if untreated.
- Chronic Kidney Disease: Long-term lithium use may cause tubulointerstitial nephritis, reducing eGFR.
- Lithium Toxicity: Polyuria increases lithium clearance, but dehydration can raise serum lithium levels, worsening toxicity.
Key Points
- Lithium causes nephrogenic DI by impairing vasopressin signaling and AQP2 function, leading to polyuria and polydipsia.
- Diagnosis: Based on history, low urine osmolality, and exclusion of other causes; water deprivation test rarely needed.
- Management: Fluid replacement, amiloride or thiazides, and possible lithium dose reduction; NDI may persist after discontinuation.
- Monitoring: Regular renal function, sodium, and lithium levels to prevent complications.
If you have specific lab values, a clinical scenario, or need recent guidelines, let me know, and I can refine the answer or search for additional data.
Disclaimer: owerl is not a doctor; please consult one.

Leave a Reply